Do you need to know more about Stemwave or Extracorporeal Shock Wave Therapy (ESWT) mechanisms and applications.
Extracorporeal Shock Wave Therapy (ESWT): Mechanisms, Applications, and Clinical Evidence in Musculoskeletal, Joint, and Spine Disorders
Introduction
Extracorporeal Shock Wave Therapy (ESWT) is a non-invasive treatment modality that utilizes acoustic pressure waves to stimulate healing processes in various musculoskeletal conditions. Initially developed for lithotripsy, ESWT has expanded its applications into orthopedics and rehabilitation medicine, offering therapeutic benefits in tendon injuries, joint disorders, and spinal pathologies.
Mechanisms of Action
ESWT exerts its therapeutic effects through several biological mechanisms:
• Mechanotransduction: The mechanical energy from shock waves is converted into biochemical signals, promoting cellular activities that facilitate tissue repair.
• Neovascularization: ESWT stimulates the formation of new blood vessels, enhancing blood flow and nutrient delivery to the affected area, thereby accelerating healing.
• Anti-inflammatory Effects: The therapy modulates inflammatory responses by downregulating pro-inflammatory cytokines, reducing inflammation and associated pain.
• Pain Modulation: ESWT may alter pain perception by affecting nerve conduction and reducing the sensitivity of nociceptors.
• Stem Cell Activation: The treatment encourages the migration and proliferation of mesenchymal stem cells, contributing to tissue regeneration.
These mechanisms collectively contribute to the regenerative and analgesic effects observed in clinical applications of ESWT.
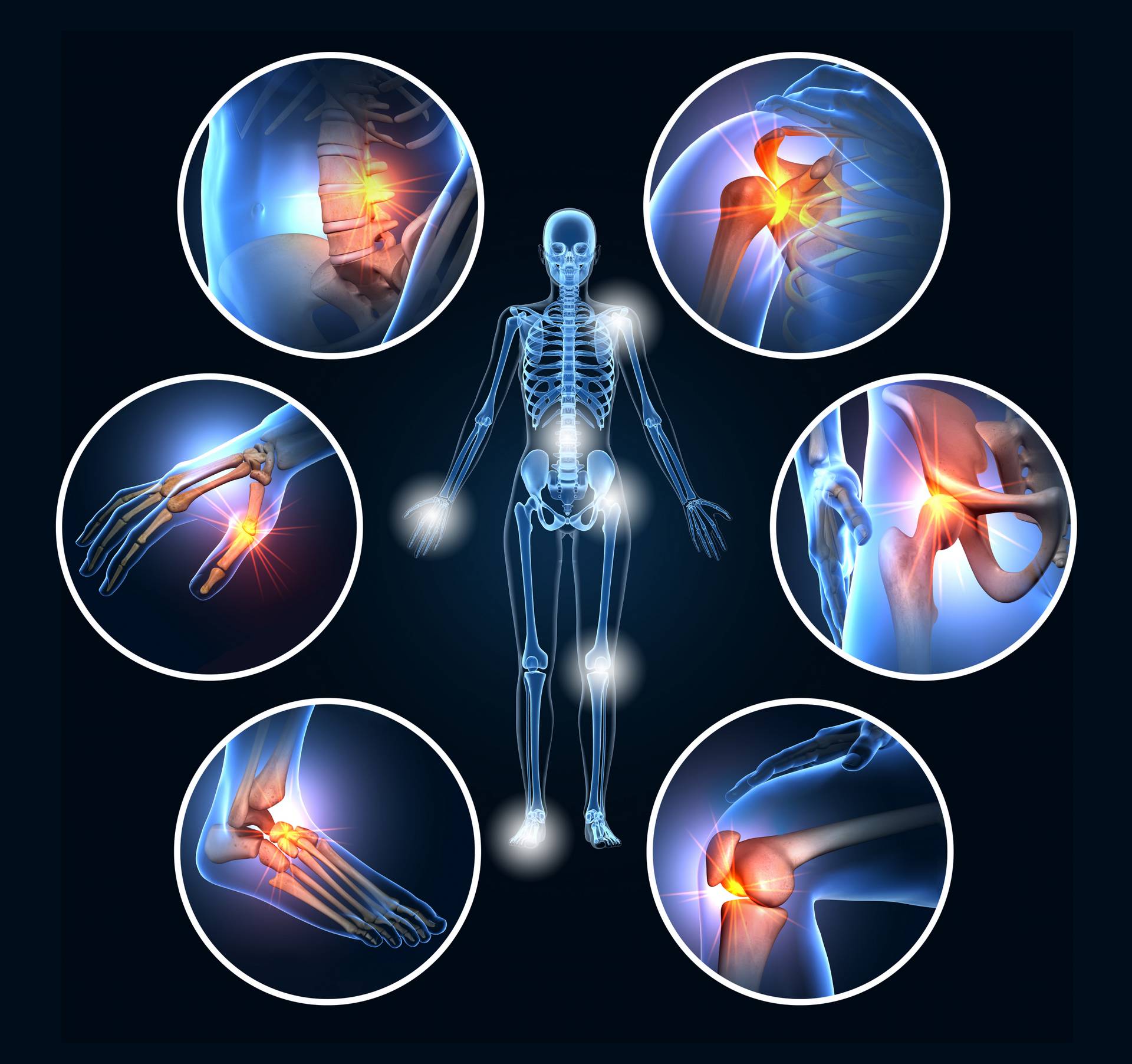
A set of six painful joints, medical 3D illustration
Applications in Musculoskeletal Disorders
ESWT has been effectively utilized in managing various musculoskeletal conditions:
• Tendinopathies: Including lateral epicondylitis (tennis elbow), Achilles tendinopathy, patellar tendinopathy, and rotator cuff tendinopathy.
• Enthesopathies: Such as plantar fasciitis, calcific tendinitis, and greater trochanteric pain syndrome.
• Bone Healing: ESWT has shown efficacy in promoting osteogenesis and enhancing callus formation in cases of delayed union or non-union fractures.
Clinical studies have demonstrated significant improvements in pain reduction and functional outcomes in these conditions following ESWT.
Joint Disorders
In joint-related pathologies, ESWT has been applied with promising results:
• Knee Osteoarthritis: ESWT has been shown to alleviate pain and improve joint function in patients with knee osteoarthritis.
• Shoulder Calcific Tendinitis: The therapy aids in the resorption of calcific deposits and reduces pain, enhancing shoulder mobility.
• Temporomandibular Joint (TMJ) Disorders: ESWT has been explored as a treatment option, with studies indicating improvements in joint mobility and pain reduction.
These applications underscore the versatility of ESWT in managing joint disorders.
Spine-Related Conditions
ESWT has been investigated for its efficacy in treating various spinal conditions:
• Chronic Low Back Pain (CLBP): Systematic reviews and meta-analyses have reported that ESWT can significantly reduce pain and improve lumbar function in patients with CLBP.
• Facet Joint Syndrome: ESWT may provide pain relief and improve mobility in patients with facet joint-related back pain.
• Myofascial Pain Syndrome: The therapy has been used to alleviate trigger point pain and muscle tension in the back.
These findings suggest that ESWT is a valuable tool in the non-invasive management of spine-related disorders.
Advantages and Limitations
Advantages:
• Non-invasive and safe with minimal side effects.
• Short treatment sessions and recovery time.
• Cost-effective compared to surgical interventions.
Limitations:
• Optimal treatment protocols (e.g., energy levels, number of sessions) are still under investigation.
• May be less effective in severe degenerative conditions.
• Contraindications include coagulopathy, local infection, and malignancy at the treatment site.
Conclusion
Extracorporeal Shock Wave Therapy represents a promising non-invasive treatment modality for various musculoskeletal, joint, and spine disorders. Its multifaceted mechanisms of action contribute to tissue regeneration and pain relief, making it a valuable addition to the therapeutic arsenal in orthopedics and rehabilitation medicine. Ongoing research is essential to optimize treatment protocols and expand its clinical applications.
References
1. Simplicio, C. L., et al. (2020). Extracorporeal shockwave therapy: Mechanisms in musculoskeletal regenerative medicine. ShockwaveNet.
2. Schmitz, C., et al. (2015). Mechanisms of shock wave therapy in musculoskeletal disorders. Bone & Joint Research, 4(3), 125–132.
3. Wang, C. J. (2012). An overview of shock wave therapy in musculoskeletal disorders. Chang Gung Medical Journal, 35(3), 197–210.
4. Kang, T. W., et al. (2020). The effectiveness of extracorporeal shockwave therapy for the treatment of knee osteoarthritis: A meta-analysis of randomized controlled trials. Medicine, 99(48), e23352.
5. Seco, J., et al. (2023). Effectiveness of extracorporeal shock wave therapy for chronic low back pain: A systematic review and meta-analysis. Journal of Orthopaedic Surgery and Research, 18(1), 198.
6. Notarnicola, A., & Moretti, B. (2012). The biological effects of extracorporeal shock wave therapy (ESWT) on tendon tissue. Muscles, Ligaments and Tendons Journal, 2(1), 33–37.


 NuVasive, Inc., the leader in spine technology innovation, focused on transforming spine surgery with minimally disruptive, procedurally integrated solutions, today announced the launch of the Pulse™ integrated technology platform. Pulse is the first, single platform to include multiple technologies designed to help surgeons adopt more efficient, less disruptive surgical approaches in all spine procedures. Engineered to improve workflow, reduce variability and increase surgical reproducibility, Pulse addresses a broader range of clinical challenges in the operating room (OR) compared to any other enabling technology in the spine market.
NuVasive, Inc., the leader in spine technology innovation, focused on transforming spine surgery with minimally disruptive, procedurally integrated solutions, today announced the launch of the Pulse™ integrated technology platform. Pulse is the first, single platform to include multiple technologies designed to help surgeons adopt more efficient, less disruptive surgical approaches in all spine procedures. Engineered to improve workflow, reduce variability and increase surgical reproducibility, Pulse addresses a broader range of clinical challenges in the operating room (OR) compared to any other enabling technology in the spine market.